Bone grafting is a common dental procedure used to rebuild parts of the jaw that have lost bone. This often happens after tooth loss, gum disease, injury, or infection.
When the jawbone becomes too thin, it may no longer support a dental implant or even nearby teeth. This can affect chewing, appearance, and overall oral stability.
Bone grafting involves placing special material in the affected area to encourage new bone growth. Over time, this restores strength and volume to the jaw, making future dental treatments possible.
At Burnaby Dentist & Orthodontist, we use digital imaging to assess jawbone health and help patients understand when grafting may be recommended as part of their treatment plan.
At a Glance:
Dental bone grafting restores lost jawbone caused by missing teeth, gum disease, or trauma. It helps improve chewing, protect facial structure, and support future dental implants. Healing is manageable with proper care, and your dentist will choose the right technique based on your needs.
Why Jaw Volume Matters
Your jawbone isn’t just there to hold your teeth—it supports your facial shape, your bite, and your long-term oral health. When bone volume is lost, it affects more than just one area.
Here’s how reduced jawbone density can impact your dental future:
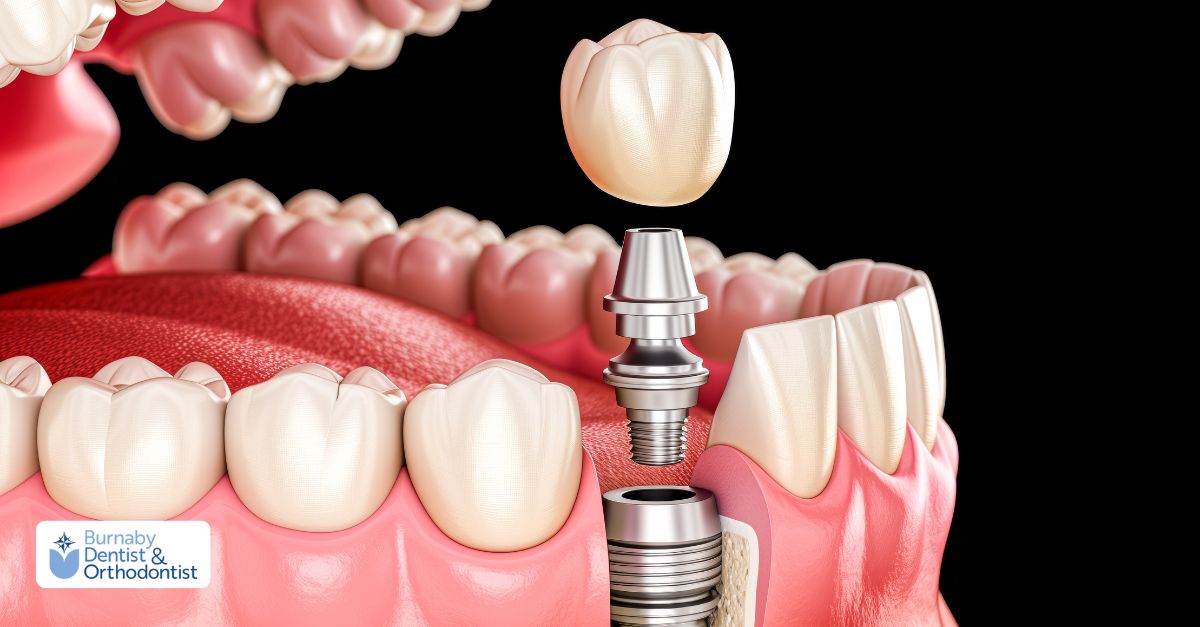
Implant Stability
Dental implants need a solid base to stay in place. Without enough bone height and width, the implant may fail to integrate properly. Read about our dental implants burnaby.
Facial Appearance
Bone loss can cause the skin around your mouth to sag or sink inward, leading to a prematurely aged or hollow appearance.
Neighbouring Teeth and Gums
As bone deteriorates, surrounding teeth lose their foundation. This increases the risk of gum recession, shifting teeth, and further tooth loss.
Bone grafting restores lost volume and helps support both the structure and function of your jaw, improving outcomes for future dental treatments.
Types of Bone Grafts in Dentistry
Different types of bone graft materials are used in dentistry, depending on your health, the area being treated, and your long-term goals. Each has unique properties and healing potential.
Autograft (Your Own Bone)
Autografts are taken from another part of your body—often the chin, jaw, or hip. Since this bone is living tissue from your own system, it’s fully compatible and naturally supports healing.
Autografts are considered the “gold standard” because they promote bone growth in three ways: they provide a structure, stimulate new cell formation, and bring live bone-forming cells to the area.
However, this approach does require a second surgical site, which can mean more recovery time.
Allograft (Human Donor Bone)
Allografts use bone from a screened human donor, typically processed and sterilized by a bone bank. These grafts support healing without needing to harvest bone from your own body.
They contain growth proteins that encourage your bone to regenerate over time. While they don’t offer live cells like autografts, they’re widely used and effective—especially in implant preparation and periodontal treatment.
Xenograft (Animal Bone)
Xenografts are derived from animal sources, usually bovine (cow). They act as a scaffold for your natural bone to grow into.
Because xenografts break down more slowly than other types, they’re ideal when long-term support is needed—such as preserving bone height after a tooth extraction.
However, they typically require a longer healing time before implant placement.
Alloplast (Synthetic Graft)
Alloplasts are made from synthetic materials like calcium phosphate or hydroxyapatite. They don’t contain any biological tissue, so there’s no risk of disease transfer or immune response.
These grafts offer structural support and are often used in smaller bone repairs. While they don’t stimulate growth as powerfully as natural grafts, they can be a safe and effective choice depending on your needs.
How Bone Grafting Works Biologically
Bone grafting doesn’t just fill a space—it helps your body rebuild bone over time. The healing process relies on three key biological mechanisms that work together to restore strength and volume.
Osteoconduction
This is the foundation of most grafts. The material acts like a scaffold, giving your body a surface where new bone cells can attach and grow. It guides the shape and structure of new bone as it forms.
Osteoinduction
In this stage, the graft releases natural proteins called growth factors. These signals tell nearby stem cells to transform into bone-forming cells, speeding up the healing and regeneration process.
Osteogenesis
This happens only with grafts that include live bone-forming cells—like autografts. These cells begin building new bone tissue immediately, making the graft more active in the healing process.
➤ Autografts support all three of these biological functions, which is why they’re often considered the most effective. Other graft types—like donor, animal, or synthetic materials—usually support osteoconduction and sometimes osteoinduction, but they don’t bring live cells to the site.
Who Might Need Bone Grafting
Bone grafting can be recommended for several reasons, especially when jawbone loss affects your oral health or limits future treatment options.
After Tooth Loss
When a tooth is missing, the surrounding bone starts to shrink over time. A bone graft placed shortly after an extraction helps preserve bone volume and maintain the shape of your jaw.
Before Dental Implants
Implants need solid bone to stay stable. If your jaw doesn’t have enough height or width to hold an implant securely, a graft may be needed to rebuild the area first.
Advanced Gum Disease
Severe periodontal disease can destroy the bone that supports your teeth. Grafting can help regenerate lost bone and prevent further damage to nearby structures.
Injury or Trauma
If you’ve suffered facial trauma or bone damage from an accident or past surgery, bone grafting can restore the structure needed for future dental work or improved function.
Congenital Conditions
In some cases, bone grafts are used to correct developmental issues—such as cleft palates or other congenital jawbone defects—especially when preparing for dental prosthetics or implants.
➤ Your dentist will examine your mouth using X-rays or 3D scans to determine whether bone grafting is the right step in your treatment plan.
What happens during a dental bone grafting procedure?
Dental bone grafting is usually performed as an outpatient procedure with local anaesthesia. The steps may vary depending on the graft location and material, but most treatments follow this general process:
1. Anaesthesia and Preparation
The area is numbed using local anaesthetic. Sedation may also be offered for patients who are anxious or undergoing a more involved procedure.
2. Incision and Cleaning
A small incision is made in the gum tissue to expose the area of bone loss. The site is then thoroughly cleaned and disinfected to prepare it for graft placement.
3. Graft Placement
The graft material is carefully inserted into the area of deficiency. Your dentist may shape it to fit the space precisely.
4. Membrane Placement
In many cases, a protective membrane is placed over the graft. This helps guide healing and keeps the graft material in place. Some membranes dissolve naturally; others may need to be removed at a later appointment.
5. Closure and Recovery
The gum tissue is repositioned over the graft and sutured closed. You’ll receive aftercare instructions and a follow-up plan to monitor healing and check graft stability.
Healing and Aftercare Tips
Recovery after a dental bone graft is usually smooth, especially when you follow your dentist’s instructions carefully. While healing times vary depending on the size of the graft and your overall health, most patients return to normal routines within a few days.
Here are some tips to support healing and reduce discomfort:
Manage Swelling
Apply ice packs to the outside of your cheek in the first 24–48 hours. This helps reduce swelling and bruising. Use 15-minute intervals on and off.
Control Bleeding
If slight bleeding occurs, apply gentle pressure with a gauze pad. Avoid rinsing aggressively or touching the area with your tongue.
Take Prescribed Medications
Follow all instructions for antibiotics or pain relievers. Don’t skip doses, even if discomfort seems minimal, as this prevents infection and controls inflammation.
Eat Soft Foods
Stick to soft, cool or lukewarm foods for the first few days. Avoid anything hard, crunchy, spicy, or hot that could disturb the graft. Sticking to a soft food diet is key after surgery, and guidelines such as What to Eat After Gum Grafting also apply to bone grafting recovery.
Maintain Oral Hygiene
Keep your mouth clean, but be gentle around the surgical site. Your dentist may recommend a medicated rinse. Avoid brushing directly over the graft until told otherwise.
Attend Follow-Ups
Your dentist will schedule follow-up visits to monitor healing and ensure the graft is integrating properly. Don’t miss these appointments—they’re essential to long-term success.
➤ Most patients experience only mild swelling and discomfort for a few days. Serious complications are rare but should be reported immediately.
Following these aftercare tips not only supports graft integration but also helps you Heal Faster After Extraction, reducing discomfort and improving recovery time.
Benefits of Bone Grafting
A well-executed bone graft doesn’t just restore missing tissue—it lays the foundation for future dental health and long-term function. Whether you’re planning for implants or preventing bone loss after an extraction, grafting offers several important benefits.
Improved Function
Bone grafting restores lost strength and volume in the jaw, making it possible to chew comfortably and speak clearly. It also provides the solid support needed for stable implant placement.
Enhanced Facial Appearance
When bone volume is lost, it can cause the face to appear sunken or aged. A bone graft helps maintain natural contours by preserving or rebuilding the underlying structure of the jaw.
Better Oral Health
By stabilizing the bone around nearby teeth, grafting prevents further bone deterioration and protects against shifting teeth, gum recession, and long-term bite changes.
Predictable Treatment Outcomes
Grafting increases the success rate of restorative procedures—especially dental implants—by ensuring there’s enough healthy bone to support them. It helps make your treatment plan more reliable and long-lasting.
Risks and Considerations
While dental bone grafting is generally safe and effective, it’s still a surgical procedure—and like any surgery, it comes with some potential risks.
Surgical Site Discomfort
Autografts, which use bone from another part of your body, may cause additional soreness at the donor site. This is temporary but may extend recovery slightly.
Infection or Bleeding
Infections are rare but possible. Some minor bleeding is expected after surgery, but prolonged or heavy bleeding should be reported to your dentist right away.
Nerve Irritation
If the graft site is close to nerves—especially in the lower jaw—there’s a small chance of temporary numbness or tingling in the lips, chin, or tongue.
Graft Rejection or Failure
Sometimes the graft doesn’t fully integrate with your natural bone. This could be due to smoking, poor oral hygiene, or systemic health issues. In such cases, a second procedure may be needed. Follow our dental hygiene services in Burnaby for oral hygiene treatments.
➤ Discuss any medical conditions, medications, or concerns with your dentist in advance. Careful planning helps reduce risks and supports a smoother recovery.
How long does it take to recover from a dental bone graft?
Healing after a dental bone graft happens in two main phases: short-term recovery and long-term integration.
Most patients feel better within a week. Swelling, tenderness, and minor discomfort usually improve during this time, allowing you to return to soft foods and light activities.
However, the bone graft itself takes longer to fully heal. In most cases, your body needs at least three months to integrate the new material. For larger or more complex grafts, full healing may take up to nine to twelve months.
Your dentist will monitor your progress through follow-up appointments and imaging to determine when you’re ready for the next step—such as implant placement or further treatment.
Final Thoughts
Bone grafting plays a key role in modern dentistry. It helps rebuild lost jawbone, support implants, and preserve facial structure—all while improving the foundation for long-term oral health.
Though it involves surgery and patience during recovery, the benefits are often well worth it. Whether you’ve lost a tooth, are planning for implants, or need to restore jaw strength after disease or trauma, a bone graft may be an important part of your treatment.
To see how bone grafting fits into our wider approach to rebuilding smiles, you can explore our restorative dentistry in Burnaby and the treatments we combine with grafting such as implants and other tooth replacement options
At Burnaby Dentist & Orthodontist, we’re here to help you explore your options with confidence. Using advanced imaging and personalized care plans, we can assess your bone health and connect you with the right treatment approach—whether that means in-house care or a referral to a specialist.
Book a consultation to learn more about your dental health, treatment possibilities, and how to protect your smile for the future.
Is bone grafting always required before getting implants?

Not always. If you have enough bone to support an implant, grafting may not be necessary. Your dentist will confirm this with imaging and clinical exams.
Will the procedure be painful?

Bone grafting is usually done with local anaesthesia or sedation. Most patients report mild discomfort after the procedure, which is manageable with medication.
What materials are used in a dental bone graft?

Grafts can be made from your own bone (autograft), donor tissue (allograft), animal bone (xenograft), or synthetic material (alloplast). Your dentist will choose the best option based on your needs.
Can a bone graft fail?

Failure is uncommon but possible. Risks include infection, rejection, or lack of integration. Good oral hygiene, not smoking, and attending follow-up visits improve the chances of success.